Tooth Erosion at the Gum Line: Causes, Treatment & Prevention
When brushing or sipping a cold beverage, have you ever experienced a sudden, sharp pain close to your gums? You find a small dip or groove that wasn’t there before when you run your tongue over your teeth. It’s easy to think, “Maybe it’s just age catching up.” But in many cases, that little notch isn’t just a sign of getting older; it’s actually tooth erosion at the gum line.
This happens when the hard outer layer of your teeth, the enamel, starts to wear away right where your teeth meet your gums. It’s more common than you might think and tends to develop slowly over time, so most people don’t notice it until their teeth become sensitive.
The good news? It’s not permanent damage if you catch it early. With a few changes to your brushing habits, diet, and dental care routine, you can stop the erosion from getting worse and even protect your teeth from future wear. Regular dental checkups and assessments, part of preventative and diagnostic care, help catch early enamel wear and prevent bigger problems later.
In this guide, we’ll break down:
- What causes tooth erosion near the gums Learn why enamel wears away at the gum line and what triggers it.
- How your dentist can treat it From fluoride varnishes to bonding, see how dental care can restore your enamel.
- Simple things you can do at home Easy daily habits to keep your smile strong and pain-free.
What Is Tooth Erosion at the Gum Line?
Tooth erosion happens when the strong outer layer of your teeth, called enamel, slowly wears away because of acid, not bacteria. It is not the same as a typical cavity. Cavities are caused by plaque and germs, but erosion is more of a chemical wearing down of the tooth surface.
When this enamel loss happens near the gums, it’s known as tooth erosion at the gum line. Dentists occasionally refer to it as a non-carious cervical lesion, which merely indicates that the tooth’s “neck”, the region where the tooth and gums meet, has lost enamel.
Along the gum line, you may see shiny, curved dips or tiny, smooth notches. The softer layer beneath, the dentin, becomes visible after persistent enamel erosion at the gum line over time. That’s when your teeth may start feeling sensitive to cold, sweets, or brushing. In more extreme cases, the area might seem a little yellow and could even lead to the tooth’s structure failing.
Common Causes of Gum-Line Erosion
Tooth erosion at the gum line doesn’t happen all at once; it’s a slow process caused by a mix of chemical, mechanical, and physical factors. The enamel, which is the hardest substance in your body, may seem indestructible, but constant exposure to acid and pressure can gradually wear it down.

Let’s take a closer look at the main causes:
1. Chemical (Acidic) Erosion
Acid is the number one reason enamel starts to dissolve, and it can come from both inside and outside your body.
Intrinsic acids (from inside your body):
Your stomach produces powerful acid to digest food. When this acid flows back into your mouth, a condition known as acid reflux or GERD (Gastroesophageal Reflux Disease), it can slowly erode the inner surfaces of your teeth.
People who experience frequent vomiting (due to medical conditions, pregnancy-related morning sickness, or eating disorders) are also at risk because every episode brings highly acidic stomach contents into contact with teeth. Dry mouth causes or a lack of saliva can make acid erosion worse.
Over time, this repeated acid exposure softens enamel, especially around the gum line, where it’s already thinner and more vulnerable.
Extrinsic acids (from foods and drinks):
These are acids that come from what we eat and drink daily.
- Soft drinks and carbonated beverages (even sugar-free ones)
- Citrus fruits like lemons, oranges, and grapefruits
- Vinegar-based foods and salad dressings
- Sports and energy drinks
- Wine and fruit juices
Even “healthy habits”, like sipping lemon water throughout the day, can be surprisingly harmful. Lemon juice has a pH around 2, which is strong enough to soften enamel after just a few minutes of contact. Knowing the best and worst foods for your teeth that protect or harm your teeth can make a huge difference. Acidic exposure can also contribute to early enamel changes, like white spots on teeth, which signal weakened enamel.
2. Mechanical (Brushing & Abrasives)
Believe it or not, brushing too hard can actually hurt your teeth, especially near the gums. Many people think scrubbing harder means “cleaner teeth,” but aggressive brushing or using a hard-bristled toothbrush can scrape away enamel over time.

When enamel has already been softened by acid (from drinks or reflux), it’s even more vulnerable. Combine that with harsh brushing or abrasive “whitening” toothpastes, and you’ve got the perfect recipe for gum-line wear.
You might start to notice small grooves or notches forming right where your teeth meet your gums. These aren’t just cosmetic issues; they can cause sensitivity and make your teeth more prone to erosion.
Learning the right brushing technique can protect enamel and gums for life.
3. Biomechanical Stress (Abfraction)
Another hidden cause of gum-line erosion is something dentists call abfraction, a fancy term for damage caused by tooth flexing.
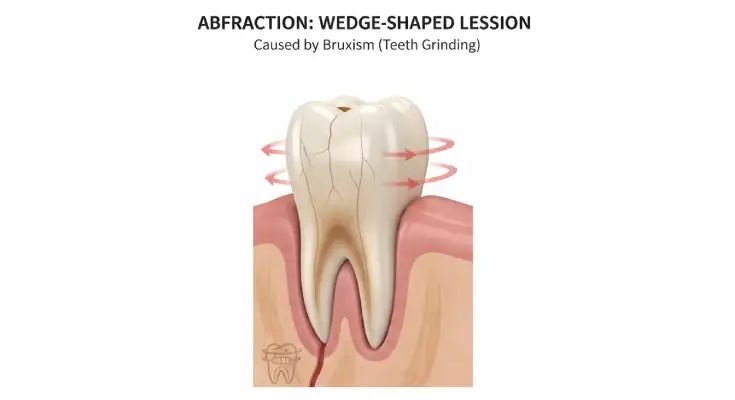
If you grind or clench your teeth (a condition known as bruxism), especially during sleep, the constant pressure causes your teeth to bend slightly at their narrowest point, right near the gum line. This repeated flexing creates tiny cracks or wedge-shaped notches in the enamel.
Over time, these microscopic stresses can cause the enamel and dentin to chip away, even if your brushing and diet are perfect. You might notice sharp sensitivity or visible grooves near your gums, often on the side teeth.
4. Other Contributing Factors
A few other things can speed up gum-line erosion or make it worse:
Low saliva flow (dry mouth): Saliva is your mouth’s natural defense. It neutralizes acids and helps rebuild minerals in enamel. Certain medications (like antihistamines, antidepressants, and blood pressure pills), dehydration, or mouth breathing can reduce saliva flow, leaving your teeth less protected. Why tooth decay aged 60 are also more prone to tooth wear and decay.
Diet and lifestyle habits: Frequent snacking, drinking acidic pre-workout drinks, or grazing on sugary foods throughout the day constantly exposes your teeth to acid. The mouth never gets time to recover its natural balance.
Aging: As we get older, gum recession becomes more common, exposing the softer root surfaces of teeth. These areas don’t have the same strong enamel covering, so they wear down faster and feel more sensitive.
How to Recognize the Signs
Tooth erosion at the gum line often starts quietly; you may not feel anything at first. But as the enamel wears away, subtle warning signs begin to show up.
Here’s what to look for:

- Shallow notches or grooves near your gums:
Run your tongue along your teeth; if you feel small dips or indentations where the tooth meets the gum, that could be early erosion. These spots may look smooth and shiny under light. - Sensitivity to cold, sweet, or acidic foods:
If sipping an iced drink or eating citrus suddenly makes your teeth twinge, it’s a sign the protective enamel has thinned, exposing the sensitive dentin underneath. - Yellowish color near the gum line:
Dentin, the inner layer beneath enamel, is naturally yellow. When enamel wears down, that yellowish shade becomes more visible, especially near the gums. - Gums that look slightly receded or uneven:
Erosion and brushing damage can make the gums pull back a bit, revealing more of the tooth’s surface. - Mild pain or discomfort while brushing:
You might feel a quick, sharp pain when your toothbrush touches the worn area, especially if you brush with pressure or use a whitening toothpaste.
How Dentists Diagnose It
If you suspect enamel erosion at the gum line, your dentist will do more than just take a quick look; they’ll try to understand what’s causing it and how far it’s progressed. Diagnosis usually starts with a few simple but thorough steps.

First, your dentist will ask about your daily habits, things like:
- What you eat and drink (especially acidic or sugary items)
- How often you brush, and what kind of toothbrush or toothpaste you use
- Whether you grind or clench your teeth, especially at night
- Any history of acid reflux, vomiting, or dry mouth
This background helps them find the root cause of the enamel loss.
Next, they’ll:
- Inspect your teeth closely under bright lighting or magnification to look for tiny notches, shiny worn spots, or wedge-shaped grooves near the gums.
- Take photographs of your teeth to monitor changes over time. These images help track whether the erosion is stable or getting worse.
- Use X-rays if needed, not always to see the erosion itself (since enamel wear can be subtle), but to check the deeper tooth structure and rule out other problems like decay or root exposure.
If your dentist suspects that acid reflux or frequent vomiting could be contributing, they might recommend seeing your physician or a gastroenterologist for a medical check-up. Treating the underlying cause, not just the teeth, is key to stopping erosion for good.
Treatment Options for Gum-Line Erosion
The good news is that gum-line erosion can be managed and even stopped, but the key is to tackle the cause, not just the symptoms. Treatment usually involves a step-by-step approach that focuses on protecting your enamel, relieving sensitivity, and restoring any lost tooth structure.
Step 1: Stop the Cause
Before any real improvement can happen, your dentist will help you address what’s causing the enamel wear.
Manage acid reflux or stomach issues:
If acid reflux (GERD) or frequent vomiting is part of the problem, your dentist may work with your physician or gastroenterologist to control the acid levels. Treating this early protects your teeth from continued erosion.Limit acidic foods and drinks:
Try to cut back on sodas, citrus juices, vinegar-based dressings, and sports drinks. If you do have them, drink them all at once rather than sipping over hours, and use a straw when possible.Rinse smart:
After eating or drinking something acidic, rinse your mouth with plain water to neutralize the acid.
⚠️ Avoid brushing right away; wait at least 30–60 minutes, because brushing too soon can scrub softened enamel away.Be gentle when brushing:
Switch to a soft-bristled toothbrush and use small, circular motions instead of aggressive side-to-side strokes. Gentle brushing is more effective and far kinder to your enamel and gums.
Step 2: Strengthen & Protect Teeth
Once the cause is under control, the next goal is to rebuild and protect what’s left of your enamel.
Fluoride treatments:
Your dentist might apply a fluoride varnish during your visit or prescribe a high-fluoride toothpaste to use at home. Fluoride helps harden and remineralize the enamel, making it more resistant to future acid attacks. Fluoride treatment for tooth decay is one of the simplest and most effective ways to strengthen enamel.Remineralizing agents (like CPP-ACP):
Products that contain casein phosphopeptide, amorphous calcium phosphate (CPP-ACP), often found in specialized creams or tooth mousses, can help restore lost minerals and strengthen early erosion spots.Desensitizing toothpaste:
If your teeth feel sensitive, use a toothpaste with potassium nitrate or stannous fluoride. These ingredients calm exposed nerves and build a protective layer over time.
Step 3: Restore Lost Tooth Structure
If erosion has caused visible notches or ongoing sensitivity, your dentist may recommend rebuilding the area with a tooth-colored filling. This helps restore the natural shape of your tooth, shields it from further damage, and provides guidance on how to treat holes in teeth if they develop. In some cases, advanced restorative options like bonding or veneers may also help restore tooth structure and aesthetics.
Resin-Modified Glass Ionomer (RMGI):
Bonds well to dentin, releases fluoride, and works well for small to moderate defects.Composite fillings:
Aesthetic and durable, these fillings blend seamlessly with your tooth color and offer strong protection.
These restorations not only improve appearance but also prevent further wear and sensitivity.
Step 4: Treat Grinding or Gum Issues
Sometimes, erosion is linked to mechanical stress or gum health problems, and those need special care too.
For teeth grinding (bruxism):
If you clench or grind your teeth, especially at night, your dentist may suggest a custom-made night guard. This protects your teeth from pressure and helps prevent new damage.For gum recession:
If the erosion has exposed your roots, a gum graft surgery might be recommended, which falls under oral surgery procedures to restore gum and tooth protection. In this simple procedure, your dentist or periodontist uses a small piece of tissue to cover the exposed area, reducing sensitivity and improving your smile’s appearance.
Home Care & Prevention Tips
Want to keep gum-line erosion from coming back? Follow this simple daily checklist to protect your enamel and keep your teeth strong and sensitivity-free.
Skip constant sipping on soda, coffee, lemon water, or energy drinks.
Have acidic drinks only with meals, and rinse with plain water afterward.
After eating or drinking something acidic, swish water around your mouth.
You can also use a mild baking soda rinse (½ teaspoon baking soda + 1 glass of water).
Wait 30–60 minutes before brushing to avoid scrubbing softened enamel.
Use a soft-bristle toothbrush and fluoride toothpaste.
Brush in gentle, circular motions, not side-to-side scrubbing.
Hard brushing = worn enamel and irritated gums.
Whitening or charcoal toothpastes often contain gritty abrasives that can damage enamel.
Choose toothpaste labeled “for sensitive teeth” or “gentle enamel care.”
Rinse with a fluoride mouthwash once a day (preferably at night).
Fluoride strengthens enamel and protects against acid wear while you sleep.
Drink plenty of water throughout the day to keep saliva flowing.
Snack on fibrous fruits and veggies, dairy, and nuts, which help neutralize acid naturally.
Conclusion
Tooth erosion at the gum line might seem minor at first, but it’s actually your mouth’s way of telling you something’s wrong. Those tiny notches or twinges of sensitivity are early warning signs that your enamel is wearing down, and the sooner you act, the easier it is to fix.
The best approach is a simple one: understand what’s causing the erosion, make small daily changes, and stay consistent with your dental care. Use a soft toothbrush, go easy on acidic foods, and visit your dentist regularly for checkups and fluoride treatments.
Taking care of your teeth now means avoiding bigger problems later. So, if you spot any sensitivity or gum-line wear, don’t ignore it, book a dental visit and start protecting your smile today.
Care at 65 Broadway Dental
At 65 Broadway Dental, we help you understand why tooth erosion happens near the gum line. We explain the causes, treatment options, and easy ways to prevent more damage. Our goal is to protect your teeth, reduce sensitivity, and keep your smile healthy.
FAQs
1. Can tooth erosion be reversed?
Minor erosion caused by the early stages of tooth erosion at the gum line can be remineralised with fluoride and calcium products, but deeper lesions require dental restoration.
2. Will fluoride fix erosion completely?
Fluoride strengthens existing enamel and protects against further wear, but it can’t replace lost enamel.
3. How long does treatment take?
Relief from sensitivity can start within a week of proper care, while full restorative treatment may take one or two dental visits.
4. Can diet changes help prevent further erosion?
Yes. Reducing acidic foods and drinks (like soda, citrus, and vinegar) and drinking more water can help protect your enamel from softening and wear.
5. Is brushing after eating acidic foods harmful?
It can be. Right after consuming acidic foods or drinks, enamel is softened. Wait 30–60 minutes before brushing to avoid scrubbing away weakened enamel.

Dr. Alexander Heifitz (Author)
Dr. Alexander Heifitz is the founder of 65 Broadway Dental in NYC, where he combines advanced dental expertise with a patient-first approach. He specializes in cosmetic and restorative treatments such as dental implants, veneers, Invisalign, and smile makeovers, helping New Yorkers achieve both oral health and confidence.
Booking An Appointment
Looking for a reliable dentist in Downtown NYC? Whether you need a routine cleaning, urgent care, or a full smile transformation — we’ve got you covered. We accept most PPO insurance plans and offer flexible scheduling.
+1 (212) 430-3888
Call for appointment
Walk-ins Welcome / Same-Day Appointments Available
Related Blogs

How to Get Rid of Bad Smell: Full Guide to Mouth, Nose, Stomach & Fresh Breath
Learn how to get rid of bad smells from mouth, nose, and stomach naturally. Easy tips for fresh breath, healthy body, and a confident lifestyle.
Read More
How to Treat Inflamed Taste Buds Fast (10+ Home Remedies That Work)
Relieve inflamed taste buds fast with easy home remedies like soothing pain, reducing swelling, and restoring your taste naturally and quickly!
Read More